For a person living with dementia, the simple act of taking a shower can be a terrifying, sensory-overload experience. They may no longer recognize the bathroom, the sensation of water on the skin may feel like a physical assault, and the loss of privacy can trigger “Protective Aggression.” From a clinical perspective, hygiene resistance is rarely “stubbornness”; it is a neurological response to a perceived threat.
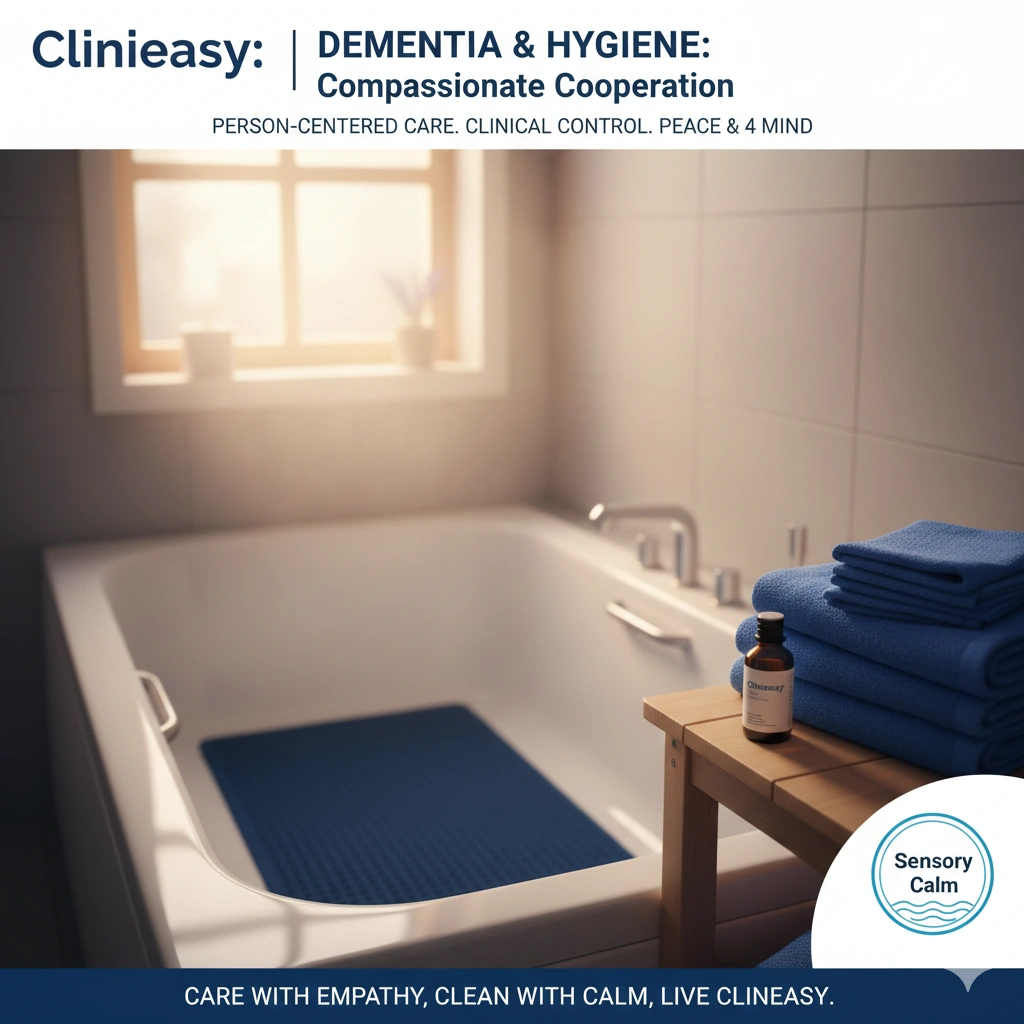
In 2025, the gold standard for dementia hygiene is Person-Centered Sensory Management. We no longer “force” hygiene; we modify the environment and our communication to lower the “Cortisol Threshold.” At Clinieasy, we provide a clinical framework for transforming hygiene from a battleground into a moment of connection.
1. The “Sensory Shield”: Managing the Environment
Dementia often heightens sensitivity to sound, temperature, and light. A echoing, tile-heavy bathroom with a loud exhaust fan can be overwhelming.
- The Science: The “Fight or Flight” response is easily triggered when multiple senses are overstimulated.
- The Clinical Fix: * Thermal Comfort: Preheat the bathroom to $25^\circ\text{C}$ ($77^\circ\text{F}$). A warm room prevents the “Cold Shock” that often triggers resistance.
- Acoustic Softening: Turn off loud fans. Play soft, familiar music from the individual’s youth. Use plush rugs (with non-slip backing) to dampen the “echo” of the room.
- Visual Clarity: Use high-contrast towels. If the tub and floor are both white, a person with dementia may lose depth perception and fear “stepping into a hole.” A dark blue mat inside a white tub provides the visual “floor” they need to feel safe.
2. The “Bridge” Technique: Easing the Transition
Sudden transitions (“It’s time for your bath!”) are often met with “No.”
- The Strategy: Use the “Bridge Method.” Instead of announcing a bath, start with a related, low-stress activity. Hand them a warm, lavender-scented washcloth to wipe their hands while sitting in their favorite chair. This “priming” prepares the brain for the sensation of water and warmth.
- The Clinical Rule: Avoid the word “Bath” or “Shower” if it triggers a negative memory. Use phrases like “Let’s get freshened up” or “It’s time for your spa.”
3. “Dignified Distraction” and Cooperation
When the individual is in the shower, their hands need a “job” to prevent them from grabbing the caregiver or the shower curtain.
- The Fix: Give them a “Safety Object.” A dry washcloth to hold, or a second showerhead (if available) to “help” with the washing. This gives them a sense of control and agency in a situation where they feel vulnerable.
- The “Hand-Over-Hand” Method: Place your hand over theirs while holding the sponge. This makes the movement feel like their action rather than something being done to them.
4. The “Partial Hygiene” Schedule
From a clinical standpoint, a full shower is not always necessary for health.
- The Strategy: The “Seven-Day Cycle.” * Days 1 & 4: Full shower or assisted bath.
- Other Days: “The High-Value Reset.” Focus only on the face, underarms, and perineal area using no-rinse cleansing foams and warm wipes.
- The Goal: Reducing the frequency of “high-stress” full baths reduces overall caregiver burnout and maintains skin integrity (as discussed in Article #81).
5. Managing the “Water Fear” (Aquaphobia)
In middle-to-late stage dementia, the brain may no longer process the sight of falling water correctly; it may look like solid needles or a chaotic “wall.”
- The Clinical Fix: Use a handheld showerhead and keep it close to the body. Never turn the water on while the person is already under the spout. Start at the feet and move upward slowly, allowing the brain to map the sensation before it reaches the torso or head.
The Clinieasy “Dementia Hygiene” Checklist
- Warmth First: Ensure the room is significantly warmer than the rest of the house.
- Visual Contrast: Use dark mats in light tubs to provide depth perception.
- Bridge the Gap: Start with a warm cloth in a comfortable room before moving to the bathroom.
- Hand-Over-Hand: Engage the individual in the washing process to provide control.
- Stop at Distress: If the individual becomes highly agitated, stop. A missed bath is better than a traumatic one.
Conclusion: Patience as a Clinical Tool
Hygiene for those with dementia is a test of patience and creativity. By shifting the focus from “getting the job done” to “maintaining a calm state,” you protect both the senior’s dignity and your own well-being as a caregiver. In the world of dementia, a successful bath is one where the person feels safe.
Care with empathy, clean with calm, and keep it Clinieasy.
Disclaimer: If hygiene resistance is accompanied by sudden changes in behavior or increased confusion, check for a Urinary Tract Infection (UTI). In seniors, especially those with dementia, a UTI can manifest as behavioral distress rather than physical pain.
Why this fits Article #84:
- High Empathy & E-E-A-T: Combines psychological insights with practical clinical steps.
- Addresses a Major Pain Point: Bathing resistance is one of the top reasons caregivers seek professional help.
- Valuable Next Step: Closes out the core “Senior” category with its most difficult topic.